Why Holiday Traditions Can Trigger Old Patterns And How to Navigate Them with Compassion
For many, the holidays are a time of joy, nostalgia, and connection, but for some, this season can be a time of stress and overwhelm. Especially individuals with trauma histories, sensory sensitivities, or ongoing stress, holiday rituals and experiences can unexpectedly pull up old patterns. Some individuals might find themselves in fight-flight-freeze mode without knowing why. These responses aren’t a moral failing. They’re normal nervous-system reactions to familiar cues that have become linked with overwhelm, stress, and/or grief.
This post explains why those reactions happen, what the nervous system is doing, and most importantly what you can do in the moment and ahead of time to regulate, reconnect to safety, and still find real moments of joy.
How holiday cues become triggers:
A “trigger” is any reminder that brings up a past painful memory or a strong emotional response. The triggers that pop up during the holidays usually fall into three broad categories:
Sensory triggers: smells (a certain perfume, freshly baked pie), sounds (carols, a loud laugh), textures (table linens, attire), and visuals (decorations, Christmas lights). Sensory cues are processed quickly and can access emotional memory before our conscious mind catches up.
Family or relational triggers: seeing a particular relative, hearing a family story, or sitting at an old seat can rekindle dynamics from the past (shame, criticism, family roles). These relational cues are powerful because early attachment experiences shape how our physiology responds to social signals.
Role-based triggers and expectations: the pressure to host perfectly, to fix relationships, or to be happy for others can revive patterns of people-pleasing, perfectionism, or overwhelm. These expectations load the nervous system and narrow our window of tolerance.
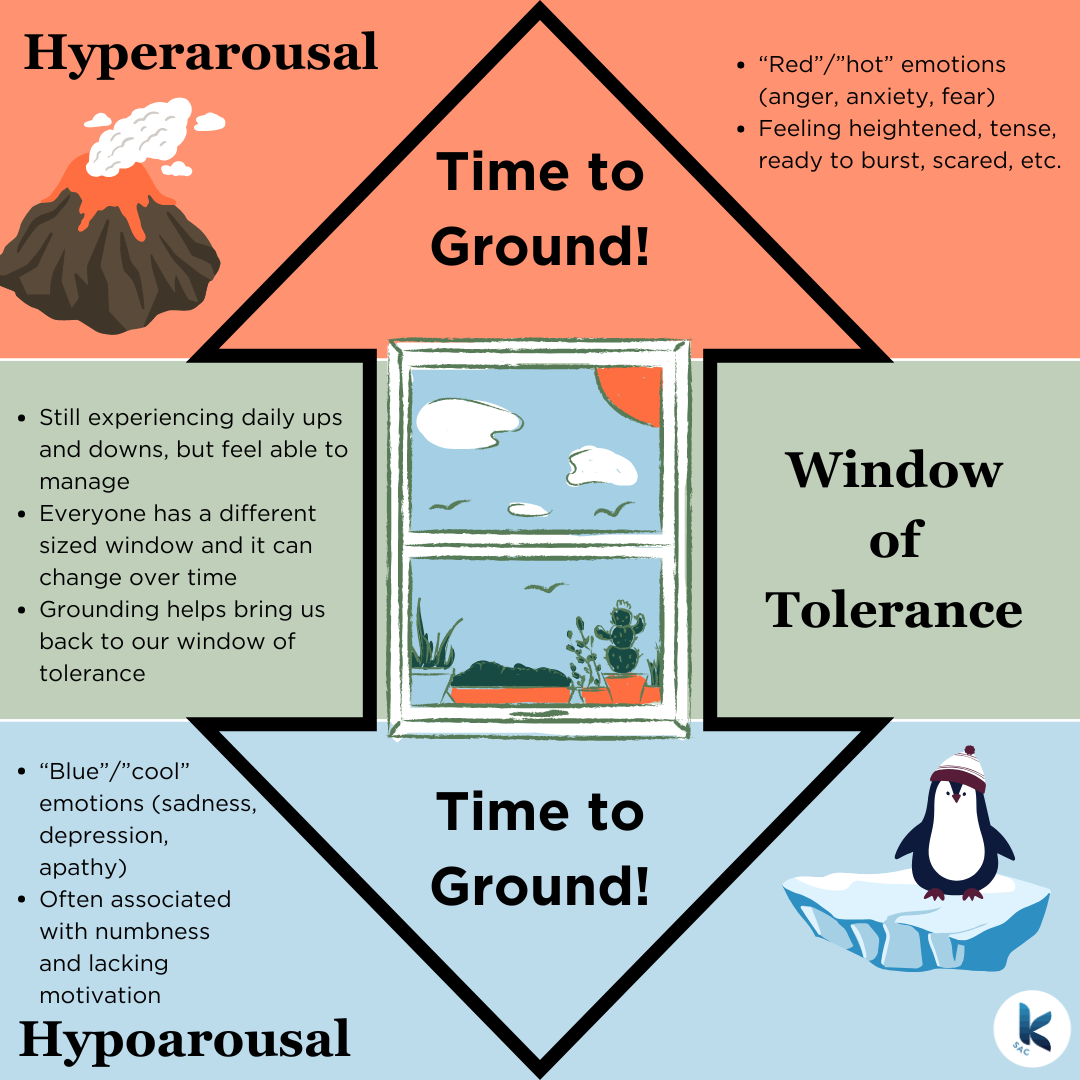
When these cues arrive in clusters (bright lights, crowded rooms, family conversation, and unrealistic expectations), they can push someone outside their window of tolerance. Window of tolerance is a term borrowed from Polyvagal Theory. It posits that we all have a range in which we can stay present and regulated. When we fall outside of this range, either on the low end (hypoarousal) or the high end (hyperarousal) we’re no longer regulated, present, and able to take care of ourselves in an effective way. That’s why someone can feel fine most of the day and then suddenly feel flooded when an old carol plays or a relative asks the “usual” question.
What the nervous system is actually doing:
The autonomic nervous system (ANS) has evolved to help us survive and connect. Modern trauma science and polyvagal theory explain how faces, voices, breathing, and social cues are tightly linked to underlying physiological states:
Polyvagal theory highlights how the ANS supports social engagement and survival. When we feel safe (ventral vagal state), we can connect, soothe, and enjoy. When cues signal danger or overwhelm, older defensive systems (sympathetic fight/flight or dorsal shutdown) come online. Those shifts happen fast and sometimes before conscious meaning. Understanding these patterns helps us respond with strategies that bring us back toward safety.
Sensory memory and PTSD research show that sensory regions can be strongly associated with traumatic memories; small sensory inputs can therefore trigger intense reactions because those inputs access slow-to-update memory networks. That’s why the scent of a dish, a tune, or a certain touch can feel like a sudden emotional avalanche.
Breath and vagal pathways: slow, intentional breathing stimulates the vagus nerve and increases heart-rate variability (HRV), a marker of parasympathetic (rest & digest) regulation. Multiple studies and systematic reviews show that slow, paced breathing (roughly 4-6 breaths per minute in many protocols) increases HRV and supports calm physiology. This is one of the quickest ways to shift the system from alarmed to regulated.
Co-regulation: humans are wired to regulate together. When another calm, attuned person is present (a partner, friend, or therapist), our physiology tends to come into alignment with theirs. Research on caregiver-child and adult attunement shows co-regulation as a robust, relational pathway back to safety. That’s why one calming presence at a gathering can make a huge difference.
Trauma-informed mindset
Before strategies, set a compassionate frame:
Your reaction makes sense. The nervous system is doing its job.
Triggers are information, not moral verdicts. They tell you where your system needs care.
Small pre-planned changes can make the difference between surviving the holiday and actually enjoying parts of it.
Practical, specific skills to regulate through the holidays:
Below are concrete, step-by-step skills you can use before, during, and after holiday events. Pick the ones that fit you and practice them once or twice so they’re accessible in the moment.
1) Before the gathering, create a coping skills plan to reduce unpredictability and lower baseline anxiety.
Make a short note of what might be triggering (e.g., loud music, my aunt commenting on my body)
Identify 2 quick exits or safe zones (a quiet bedroom, outside porch).
Pack a small regulation kit: noise-reducing earplugs or headphones, a fidget or stress ball, a bottle of lavender-scented hand lotion, a note with self-soothing reminders.
Share the plan with a trusted person who can support you if needed.
2) Grounding exercise: 5-4-3-2-1 to anchor you in the present when overwhelm spikes.
Name 5 things you can see.
Name 4 things you can touch.
Name 3 things you can hear.
Name 2 things you can smell
Name 1 thing you can taste
Do this slowly and notice the body as you move through it.
3) Breath skill: Box Breathing (4-6 breaths per minute) to engage vagal pathways and increase HRV.
Sit comfortably. Place one hand on your belly.
Inhale gently for 4 seconds (feel the belly rise).
Hold the breath for 4 seconds.
Exhale for 6 seconds (longer exhale).
Hold the breath for 4 seconds.
Repeat for 4-5 minutes or until you feel more grounded.
4) Micro-movement for regulation (30-60 seconds) to discharge built-up activation without needing to leave the room.
Stand and shift weight gently side to side, march in place, shake hands, or do subtle shoulder rolls.
Pair with breathing: inhale for the movement, exhale and release tension.
Even brief movement changes the autonomic balance.
5) Co-regulation scripts: How to ask for help
To a friend: “I’m noticing I’m getting overwhelmed, would you sit with me outside for five minutes?”
To a partner: “Can you hold my hand for a minute? I need to slow my breathing.”
To family: “I love being here, but I need a short break. I’ll be back in 15 minutes.”
Asking for co-regulation gives you access to another person’s calmer nervous system
When to seek professional help
If holiday triggers lead to repeated nights of insomnia, flashbacks, or difficulty functioning, consider reaching out to a therapist with trauma-informed training. Structured therapies and guided practices can help expand the window of tolerance and reduce the intensity and frequency of triggers.
While the holidays may trigger a time of stress and overwhelm, it doesn’t mean that it will be this way forever. With each moment of self-regulation, you build resilience and your ability to tolerate increase stress without falling into old patterns. Each time you do fall into an old pattern of behavior, guilt, people-pleasing, etc., have grace with yourself. Healing requires patience and self-compassion. The more you honor your needs in each moment and recognize that your reactions are your neurobiology protecting you, the more you will be able to take the necessary steps to heal and enjoy the true meaning of the holidays.
From the cypress team, we wish you a peaceful holiday season.
If you or someone you know is struggling with their mental health, reach out for help today. At Cypress Wellness Collective, we can help. Cypress Wellness Collective is located in the San Francisco Bay Area where they specialize in therapy, nutrition counseling, and KAP for teens, adults, and families going through mental health challenges, including depression, anxiety, and eating disorders. They offer in person and virtual appointments throughout all of California. Call today for your free consultation to see if Cypress Wellness Collective is right for you!
References:
Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. W. W. Norton.
Substance Abuse and Mental Health Services Administration. (2014). Understanding the impact of trauma. In Trauma-informed care in behavioral health services. Substance Abuse and Mental Health Services Administration.
Fleming, L. L., Boyd, J. E., & McKinnon, M. C. (2023). Sensory alterations in posttraumatic stress disorder: A review of neural, perceptual, and clinical perspectives.PMC Article
Laborde, S., Mosley, E., & Mertgen, A. (2022). A systematic review of the effects of slow-paced breathing on heart rate variability and emotional regulation.
You, M., Laborde, S., & Dosseville, F. (2021). Effects of slow-paced breathing on heart rate variability and stress: A randomized controlled study.
Lunkenheimer, E., Tiberio, S. S., Skoranski, A. M., Buss, K. A., & Lucas-Thompson, R. G. (2017). Dyadic coregulation and child–caregiver physiology: A systems view of early development.